Nonheterosexual couples sue state of New Jersey for discrimination
 Horizon Blue Cross Blue Shield recently refused to cover fertility treatments for lesbian couple Sarah Mills and her wife Gloria Torres. The reason: “Because I did not have sexual intercourse — as mandated by the state — with a man, for two years. I was appalled,” said Mills.
Horizon Blue Cross Blue Shield recently refused to cover fertility treatments for lesbian couple Sarah Mills and her wife Gloria Torres. The reason: “Because I did not have sexual intercourse — as mandated by the state — with a man, for two years. I was appalled,” said Mills.
The state of New Jersey is one of 15 states that requires most major health insurance companies to cover fertility treatments. The state mandate requires that couples demonstrate their infertility through “two years of unprotected sex.” The wording of the mandate is not inclusive for nonheterosexual patients, giving them no way to qualify as infertile.
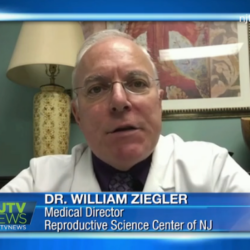
“The majority of insurances will deny coverage for same-sex relationship couples and the reasons they give is because they have not been exposed to sperm for the length of time in which their policy describes. I feel that the insurance companies need to readdress the definition of how they define infertility because our society is changing and they need to change with it,” said Dr. William Zeigler, Medical Director of the Reproductive Science Center of New Jersey.
Fertility experts such as Dr. Zeigler see issues with health insurance companies covering fertility treatments frequently. Same-sex couples in New Jersey such as Sarah Mills and Gloria Torres will have to pay for fertility treatments by themselves for now. Meanwhile, there is a bill being pushed through that would fix the wording in the state insurance mandate, and nonheterosexual couples in New Jersey are also pursuing legal action.
