In Vitro Fertilization (IVF)
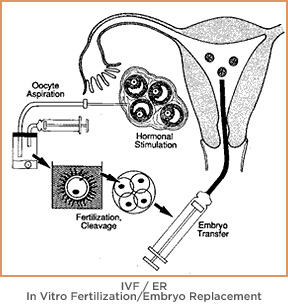
In vitro fertilization (IVF) fertility treatment involves combining a female egg with male sperm in an IVF laboratory to promote fertilization resulting in an embryo that can be transferred to the woman’s uterus for a pregnancy. IVF is the most successful and advanced form of assisted reproductive technologies (ART).
This treatment is utilized in more difficult infertility cases involving:
- Blockage of both fallopian tubes.
- Male factor infertility.
- Severe endometriosis.
- Pelvic adhesions.
- A diagnosis of unexplained infertility.
- Problems that cannot be corrected with other treatments.
IVF is a necessary reproductive treatment for many LGBTQ+ individuals or couples who wish to have a biological family of their own.
Why we use assisted reproductive technologies
We use assisted reproductive technologies (ART) like IVF when an infertile couple cannot be treated using simpler methods or when all other methods have failed. These procedures have excellent success rates but require a significant amount of time, effort and, in some cases, money.
Our team helps to minimize these added pressures by explaining each process fully and answering all patient questions so they understand exactly what is required of them for these types of therapies to be successful.
Improvements in ART knowledge and technological advances have increased the number of infertile couples and LGBTQ+ patients achieving pregnancy. According to the Centers for Disease Control and Prevention’s latest data, about 2.3% of all births in the United States are conceived through ART.
The original and most often used infertility therapy is in vitro fertilization, which, along with other techniques, has substantially increased the likelihood of couples having babies. Reproductive Science Center of New Jersey offers all of the assisted reproductive technologies available worldwide.
The IVF process is complex and is often successful due to laboratory practices ensuring that the egg and sperm make contact to create an embryo and controlled placement of the embryo in the mother’s womb. Both steps are often problematic in natural conception.
IVF consists of several steps, including: ovulation induction, egg retrieval surgery, fertilization of the eggs, embryo development in a controlled culture, embryo grading and embryo transfer. These steps are addressed in detail below.
Learn how reciprocal IVF can help lesbian couples share in the IVF process.
The IVF process first step: ovulation induction
Hormone injections are given to stimulate multiple egg production. Normal ovulation generally results in one egg being released, but retrieving multiple eggs in IVF improves the chances of successful fertilization and implantation, as well as often resulting in eggs and/or embryos to preserve and use in the future.
This stimulation process usually requires the initial use of Lupron to suppress the ovary to prevent ovulation or the use of Antagon or Cetrotide during the stimulation cycle until the desired time. Daily gonadotropin injections are then added to stimulate the development of the eggs.
These are usually given subcutaneously (under the skin) and are generally well tolerated. We then monitor the progress of ovulation induction with ultrasounds and blood estrogen levels over several days.
Is minimal stimulation IVF right for you?
Minimal stimulation IVF, or mini IVF, uses fewer drugs at the stimulation and possibly the egg retrieval process. We can help you determine if lower-cost mini IVF is right for you.
Egg retrieval
Egg retrieval is minimally invasive surgery performed by placing a special needle into the ovarian follicle and removing the fluid that contains the egg. This is a relatively minor procedure and is performed by visualizing the follicles with a vaginal ultrasound probe. A needle is directed alongside the probe, through the vaginal wall and into the ovary. To avoid any discomfort, strong, short-acting intravenous sedation is provided.
Egg fertilization
Once the follicular fluid is removed from the follicle, the eggs are identified by the embryologist and placed into an incubator. The eggs are fertilized with sperm later that day by conventional insemination. This involves placing approximately 50,000 sperm with each egg in a culture dish and leaving them together overnight to undergo the fertilization process.
Intracytoplasmic sperm injection (ICSI)
Sometimes we use intracytoplasmic sperm injection (ICSI) to fertilize mature eggs in the event of sperm or egg abnormalities. Under the microscope, the embryologist picks up a single sperm and injects it directly into the cytoplasm of the egg using a small glass needle. The cytoplasm is where fertilization occurs.
ICSI allows couples with very low sperm counts, poor quality sperm or women whose outer egg shell (zona pellucida) is too thick for sperm to penetrate to achieve fertilization and pregnancy rates equal to traditional IVF. It is also recommended for couples who have not achieved fertilization in prior IVF attempts or if a low number of eggs are retrieved (< 5).
IVF embryo grading & quality
The grading of embryos has two purposes: First is to determine the number of embryos that should be transferred to avoid a multiple pregnancy (twins or more), and second is to decide if the remaining embryos are of good enough quality for cryopreservation. The quality of an embryo is determined by assessing three major components: cell number, cell regularity (regularity of size) and degree of fragmentation.
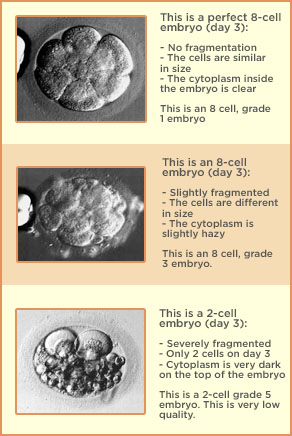
The determination of “quality” is not made until about 48 hours after the egg retrieval. By 48 hours good quality embryos should be at least four cells. If they are not at least two cells by then, they are considered “arrested” and should not be transferred. By 72 hours after retrieval, we prefer that some of the embryos are at least 6-7 cells.
Embryos with higher cell numbers and regular appearing cells, called blastomeres, and little or no fragmentation have a higher overall chance of implanting than do embryos with less cells, more irregularity and more fragmentation. Embryo quality gives us information to predict the chances of pregnancy from an embryo transfer.
The grades of the embryos have no relationship to birth defects, intelligence, strength or athletic ability. The only difference as far as we know is in the chance that the transfer of the embryo(s) will result in a pregnancy and a live birth.
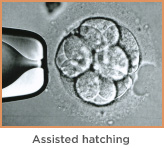
Assisted hatching & IVF
During assisted hatching, which usually takes place on day 3 of embryo development, the embryo’s zona pellucida is opened using micromanipulation. This helps the embryo to shed its outer coating and in certain cases improves implantation and pregnancy rates.
The opening in the shell is performed using a chemical or laser technology. A very small opening is made to facilitate embryo hatching. This procedure is very quick and can be completed in less than half-a-second.
This technique is beneficial for older women and for women who previously have not achieved pregnancy with IVF.
Blastocyst development
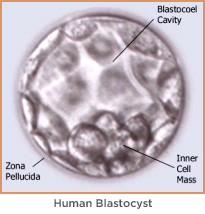
Whether or not ICSI is used, the eggs will be checked to document fertilization the following day and again the next day to evaluate for early cell division. After fertilization they are called embryos and are placed in a solution called embryo culture medium, which is a nutrient rich solution that promotes growth.
On day 2 or 3 after fertilization, the embryos will be evaluated for blastocyst culture. If there is a sufficient number of dividing embryos, they will be placed in special blastocyst media and grown for two or three additional days.
If possible, we prefer to grow the embryos for five days until they reach the blastocyst stage — the point at which, during natural conception, embryos arrive in the uterus. By delaying the blastocyst transfer a few extra days, fertility specialists are much better able to select the embryos that have the best chance for survival.
In turn, by growing embryos to a more advanced stage, fertility physicians are able to transfer fewer embryos without decreasing the chance for pregnancy. This advancement maintains a high pregnancy rate while decreasing the risk of conceiving a high-order multiple pregnancy – helping avoid serious risks to both the mother and baby.
Preimplantation genetic testing (PGT) during IVF
We can conduct this form of testing only on IVF embryos created in the lab before being implanted in the womb. PGT can detect the presence of genetic or chromosomal defects that can cause embryo implantation failure, miscarriage or birth defects in a resulting child. This can be a good idea for couple or individuals with risk of passing along an inheritable genetic condition, as well as for older mothers whose eggs are more likely to have genetic problems.
Embryo transfer
Embryos may be transferred on day 2, 3 or 5 after egg retrieval. As mentioned above, we prefer to transfer on day 5 when the embryo is at the blastocyst stage. Embryos are placed through the cervix into the uterine cavity using a small, soft catheter.
Because the implantation process is a complex one, there are many other contributing factors we cannot measure. We have seen the two extremes from a failed cycle with the transfer of three perfect looking embryos to a successful pregnancy with transferring one low grade embryo.
The embryo transfer is an important variable that could affect the implantation process. Knowing the uterine length by passing a practice catheter is critical so the embryos could be placed correctly in the uterus. At the time of the embryo transfer, an ultrasound is sometimes used to confirm the correct placement of the embryo transfer catheter.
When the catheter containing the embryos is passed, it should occur in a smooth fashion without trauma to the endometrial lining. This would give the embryos the best chance for implantation and normal development.
Embryo transfer usually requires no anesthesia.
After the embryo transfer
Progesterone is routinely given to support the uterine lining and could be given by an injection or vaginal application. This is continued until 10-12 weeks of pregnancy. At that time the placenta should be competent to make its own progesterone to maintain the pregnancy.
In those patients who did not have an optimal response or if the embryology is poor, we give estrogen in a pill form to enhance implantation. A blood test is performed 12 days after the embryo transfer to confirm a pregnancy.
We welcome all patients, even those with difficult cases. We’re proud of our IVF success rates, but we’re more proud of helping everyone have a family.
Read, download or print the IVF Handbook


